1. As you consider the issues regarding fatigue and technology-mediated practice, what things occurred to you prior to reading these articles? Was this based on personal experience, experiences of others you knew, or your own understanding of technology-mediated practice?
Before reading the articles, I already had some sense that technology-mediated practice could lead to fatigue and burnout. This was mostly from my own experiences and what I’ve noticed from colleagues in helping professions. I’ve felt how back-to-back virtual meetings, constant notifications, and long hours on a screen can be mentally exhausting, even when the work itself is meaningful. I’ve also seen friends or coworkers mention feeling “always on” when working from home, which makes it harder to disconnect and recharge. So, even though technology makes things convenient, it definitely comes with challenges for maintaining energy and focus.
2. In looking at the continuum from health to burnout in Hilty, et.al, Fig 2, which of the four areas resonated most with you? Why? How would you prevent moving from health to burnout in that area?
The area that really stood out to me was the shift from moderate stress to high stress, where emotional exhaustion starts to set in. That hit home because I’ve felt that overwhelm before, when client needs or deadlines pile up and my energy just dips. To prevent burnout in that area, I would focus on keeping a routine that includes short breaks, clear boundaries around work time, and regular check-ins with peers or supervisors to share the load. I think intentionally scheduling moments to recharge, even briefly, would make a big difference in staying balanced.
3. In Table 2 of Hilty, et.al., they discuss the human factor related to tech fatigue. Select one issue in each of the four areas (tech and office, training, clinical care, human factors) and talk about how you might face that issue personally and how you would most likely address it to prevent tech fatigue.
For tech and office, poor ergonomics stood out because I know sitting at a desk for hours can be rough on the body. I’d make sure my workspace is set up properly with a supportive chair and monitor at eye level to reduce strain. For training, I could see myself struggling if I didn’t fully understand new tech tools. I would fix that by looking up tutorials or asking a coworker for guidance until I felt confident. In clinical care, doing too many virtual sessions in a row could make me emotionally drained, so I’d try to schedule breaks between sessions and practice grounding techniques to stay present with each client. For human factors, blurring work and personal life feels familiar. I’d combat this by setting clear start and stop times, turning off notifications after work, and letting clients know when I’m available.
4. When you read the opinions of the clinicians in the MacDonald article, which reactions resonated for you? Why? Do you see yourself engaging in remote, technology-mediated practice? Why or why not?
I really connected with the clinicians who talked about struggling to separate work and personal life while working from home. That has been a challenge for me too, and I know it can make it hard to “switch off” at the end of the day. I could see myself doing some remote work because it can be flexible and helps reach clients who can’t come in person, but I’d want to balance it with in-person work. Too much screen time can be draining, and I’d want to make sure I’m still building meaningful relationships with clients without burning out.
5. Ratcliff provides a definition of burnout and also some suggested solutions for self-care. What did you think of her definitions of burnout? Did they seem accurate in your experience? She mentions a number of studies and writings. Did you feel motivated to read any of them? Why? Have you ever taken the MBI (Maslach Burnout Inventory)? Would you like to? Why?
I thought Ratcliff’s definitions of burnout were really accurate. Emotional exhaustion, depersonalization, and feeling less accomplished really match what I’ve seen in myself and others. The physical and emotional impacts she described made me realize how serious burnout can be. Her references to studies on self-care interventions made me curious to read more, especially to see practical strategies I could actually use. I haven’t taken the Maslach Burnout Inventory yet, but I think it would be helpful to see where I might be at personally and identify areas to focus on before burnout gets worse.
6. Did you think any of the suggestions Ratcliff provided were useful in preventing burnout? If not, why not? What other suggestions do you think she could have included?
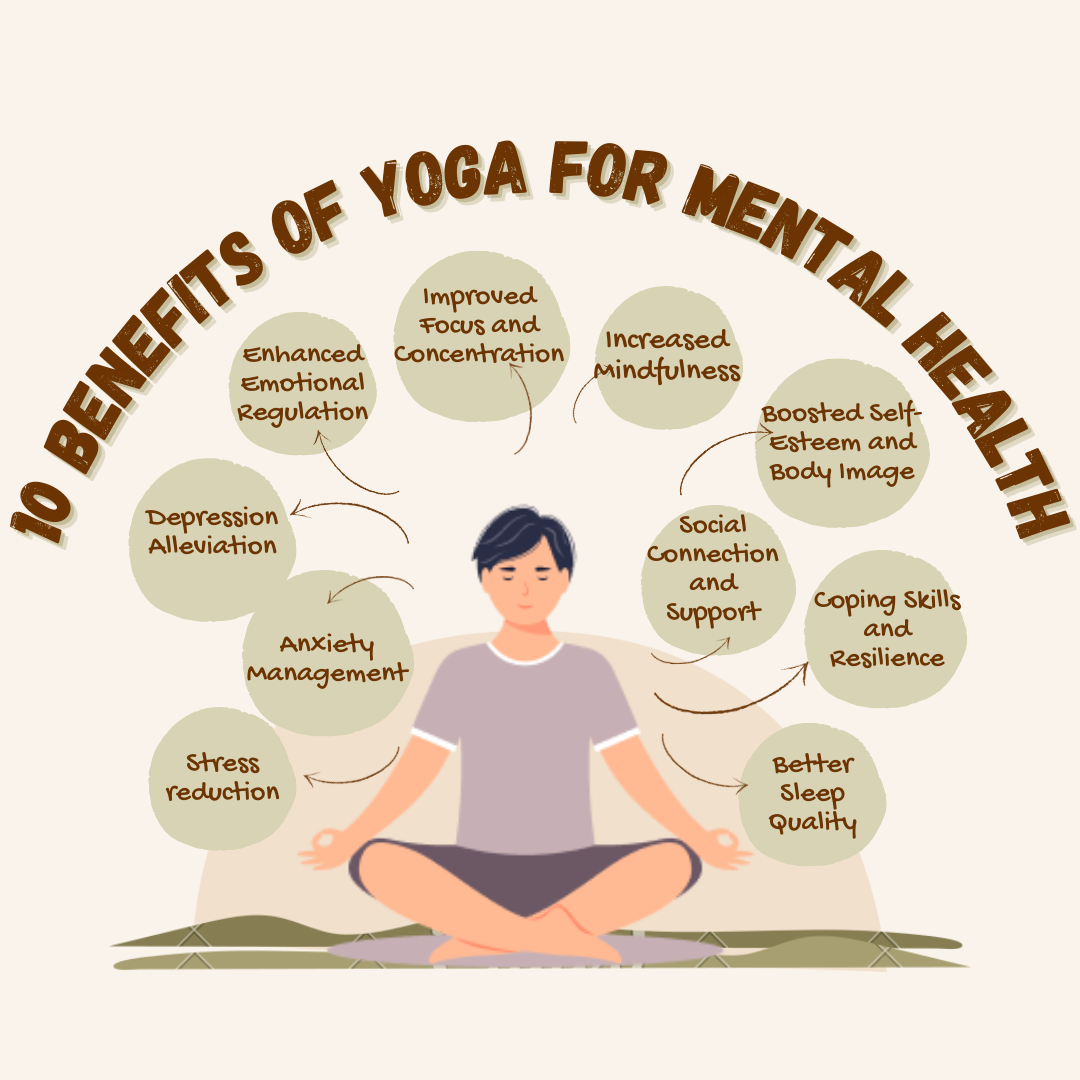
I thought her suggestions, like mindfulness and yoga, were really useful because they address both the mental and physical aspects of stress. I like that these practices encourage being present and aware, which can help manage stress in real-time. I think she could have added strategies for better time management, delegation, and peer support, since sharing the workload and having a support system can also prevent burnout. Organizational policies, like encouraging breaks, limiting caseloads, or providing mental health resources, would also be great additions to help social workers take care of themselves.
Korie,
This was a good post and I appreciated your ideas on managing the stress of technology-mediated practice. Just an FYI, if you put your image in the “set featured image” section (at the bottom of the post writing screen, under the menus where is say to set the image) then we can all see it right at the top of your post. This was a great image and we didn’t miss it, but it would be nice to lead with that.
I think your last answer was your best one. When we talk about eating breaks, having good self-care habits, managing workload, those are often things that are out of our individual control. Organizational policies are going to be essential in making that happen.
Good job.
Dr P